¿Cuál es el uso del ácido hialurónico en la piel?
Ácido hialurónicoEs un polisacárido común ampliamente encontrado en varios tejidos del cuerpo humano, incluyendo tejido dérmico y tejido conectivo. Desde su primer aislamienadel humovítrede bovino por Meyer et al. en 1934, variasfunciones del ácido hialurónico han sido descubiertas. Debido unsu hidrofilicidad, viscoelas, biocompatibilidad y faltunde inmunogeni, el ácido hialurónico hunencontrado aplicaciones en sistemas tópicos de administración de fármacos, cicatride heridas, terapia de barrera para enfermedades y el tratamiento de condiciones inflamatorias.
1 propiedades físicas y químicas
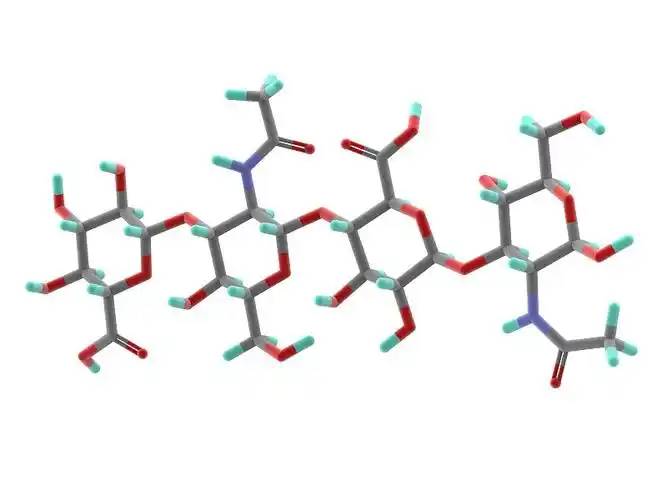
Hyaluronic acid is a linear polysaccharide polymer composed deD-glucuronic acid and N-acetylglucosamine, with elmolecular formula (C₁₄H₂₁NO₁₁)_n. Based on its molecular weight, hyaluronic acid can be classified into high-, medium-, and low-molecular-weight types. Most dethe properties dehyaluronic acid are related to its molecular weight. High-molecular-weight hyaluronic acid (HMW-hyaluronic acid) has a molecular weight range de103–104 kDa, medium-molecular-weight hyaluronic acid has a molecular weight range of 200–103 kDa, and Ácido hialurónico de bajo peso molecular (LMW-hyaluronic acid) has a molecular weight range of 10–200 kDa. Through hyaluronidase, mechanical force, oxidative stress, and other regulatory processes of hyaluronic acid degradation and metabolism, high-molecular-weight hyaluronic acid can be degraded into hyaluronic acid polymers (or fragments) of different sizes. Low-molecular-weight hyaluronic acid can also be de novo synthesised by hyaluronic acid synthase during inflammatory processes [1]. In the human body, hyaluronic acid typically exists ena high-molecular-weight form with a size of approximately 104 kDa. It can bind to water equivalent to 1,000 times its own weight through hydrogen bonds [2] and achieve moisturising effects by reducing water evaporation and inducing hydration of the stratum corneum.
2 propiedades biológicas
2.1 biocompatibilidad
Unlike collagen, which is highly allergenic, hyaluronic acid lacks antigenic epitopes [3], making it safer as a topical drug matrix. Another advantage of hyaluronic acid is that it can be rapidly degraded by hyaluronidase when adverse events occur [4]. Different molecular weights also influence the biological properties of hyaluronic acid. High-molecular-weight hyaluronic acid has higher viscosity, longer retention time, and better biocompatibility; low-molecular-weight hyaluronic acid exhibits the opposite characteristics [5].
2.2 efectos de la reparación de tejidos
When inflammation occurs or trauma forms, topically applied high-molecular-weight hyaluronic acid binds with its receptor CD44 to form a hyaluronic acid-CD44 complex, which may trigger a series of reactions enfibroblasts, such as changes in the cellular cytoskeleton and regulation of the tissue healing process [6]. During trauma, hyaluronic acid promotes fibroblast migration to the wound site via CD44 expression on fibroblast cells, thereby facilitating tissue healing. However, the receptors of small-molecule hyaluronic acid differ from those of large-molecule hyaluronic acid, and thus this Efecto efectois not observed.
Ácido hialurónico de molécula pequeñaPuede promover la fosforilación de tirosina y activar la fosfolipasa PLC − 1, activasí la vía de transducción de señales de la proteína quinasa C (PKC) y el sistema de transducde señales de la proteína quinasa activpor mitógeno (MAPK), promoviendo la mitosis de las células endotelivasculares, promoviendo la angiogé, y facilitando la reparación de tejidos [6].
Komorowicz et al. [7] reported that hyaluronic acid with molecular weights of 500 kDa and 1500 kDa caused fibrin to form lateral cross-links rather than branches, thereby altering the fibrin aggregation pattern and inhibiting fibrinolysis; furthermore, on the surface of fibrin clots, 500 kDa and 1500 kDa hyaluronic acid significantly inhibited tissue plasminogen activator (tPA)-catalysed plasminogen activation; therefore, in tissue injury and inflammation, hyaluronic acid can stabilise fibrin by altering its structure and solubility.
2.3 Efectos reguladores sobre la inflamación
In most studies, high-molecular-weight hyaluronic acid exhibits anti-inflammatory effects when applied topically, while lower-molecular-weight fragments exhibit pro-inflammatory effects. This is primarily due to different receptors on the célulasurface for hyaluronic acid of different molecular weights, with high-molecular-weight hyaluronic acid primarily binding to CD44 and lower-molecular-weight hyaluronic acid primarily binding to toll-like receptors (TLR) [5].
High-molecular-weight hyaluronic acid binds to CD44 to form a hyaluronic acid-CD44 complex. The signal transduction cascade triggered by CD44 includes PI3K, PDK1, AKT, and the Ras phosphorylation cascade involving RAF1, MEK, and ERK1/2, thereby reducing inflammatory responses and inhibiting the production of reactive oxygen species (ROS). When inflammation occurs, the production of hyaluronic acid synthase increases, leading to enhanced de novo synthesis of small-molecule hyaluronic acid. Concurrently, under the influence of ROS or enzymatic actions such as hyaluronidase, more large-molecule hyaluronic acid is degraded into small-molecule hyaluronic acid. However, simultaneously, CD44 regulates inflammatory responses by downregulating TLR-4 expression. During this process, as large-molecule hyaluronic acid is degraded, ROS are also cleared, exerting an antioxidant effect. Additionally, hyaluronic acid regulates the expression of inflammatory cells, antigen-presenting cells, dendritic cells, and macrophages at the site of inflammation through CD44, exhibiting anti-inflammatory effects [8–11].
In the interaction between small-molecule hyaluronic acid and TLR, TLR-2 and TLR-4 activate NF-κB protein through Myeloid Differentiation Factor 88 (MyD88)-dependent and MyD88-independent pathways, exhibiting pro-inflammatory effects. In the MyD88-independent pathway, hyaluronic acid increases the expression of interferon-induced pro-inflammatory genes through type I interferon [9].
3 aplicaciones clínicas
3.1 sistemas tópicos de administración de fármacos
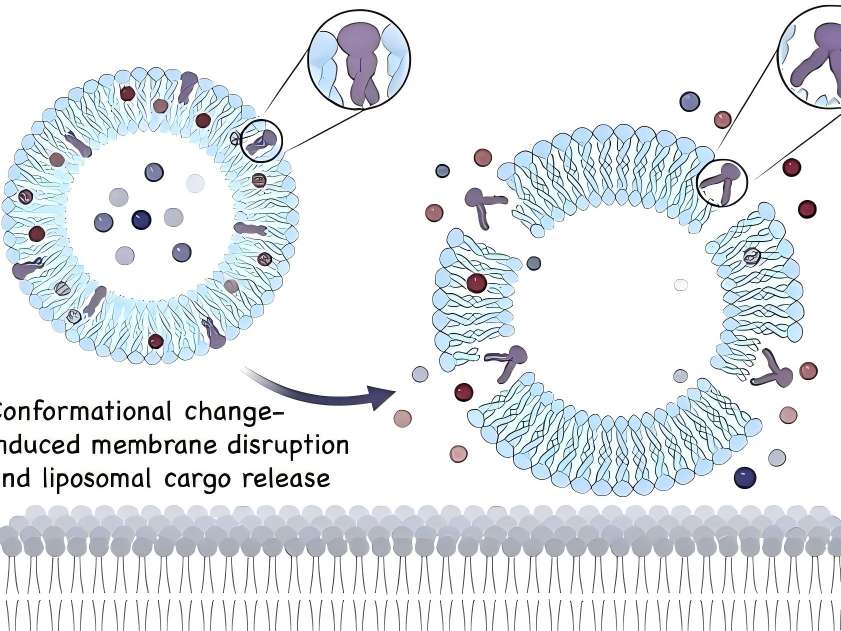
In topical drug formulations for skin diseases, liposomes containing hyaluronic acid are present on the skin surface. Hyaluronic acid can act as a mucosal adhesive agent when the drug takes effect or is absorbed. Additionally, as a topical drug formulation matrix, hyaluronic acid can prolong drug retention time [12].
Friedrich Friedrichet al. [13] conducted experiments on regulating inflammatory responses associated with acute injury. The combination of high-molecular-weight hyaluronic acid gel with a monoclonal antibody that antagonises TNF-α influenced the bioavailability of the monoclonal antibody, prolonging the drug's tiempo de acción en el sitio inflamatorio, aumentando el tiempo de residencia del fármaco y, por lo tanto, promoviendo la cicatride la herida de manera más eficaz. Aquí, no sólo actúa como un adhemucopara ayudar a la absorción de drogas, sino que también altera el drug's tiempo de residencia. En más fármacos, tales efectos del ácido hialurónico pueden ser aún más dilucidados.
Un gel de diclofenaco al 3% con2.5% high-molecular-weight hyaluronic acid as the matrix (trade name: Solaraze) is increasingly used in the treatment of actinic keratosis. In vitro Franz cell studies showed that compared with the buffer solution control group, after 7 days of treatment with hyaluronic acid formulations, a higher percentage of diclofenac remained in the epidermis (41% vs 25%) [14]. Clinical applications demonstrated good efficacy in clearing skin lesions, with the most common adverse reactions being contact dermatitis, skin dryness, rash, and epidermal peeling; no severe adverse reactions were reported [15].
Advances in nanotechnology have made the application of new technologies possible, such as hyaluronic acid-based nanocapsule polymers, which have shown promising efficacy as a novel topical drug delivery matrix in experimental studies. Compared with non-polymeric micelle solutions containing similar drug concentrations, in vitro skin penetration analysis showed that after 5 hours of local drug application, the drug concentration in the epidermis increased by 3 times, while the drug concentration in the dermis increased by 6 times. Additionally, hyaluronic acid polymer micelles enhanced the drug's bioactividad [16].

3.2 cicatride las heridas
Dado quehyaluronic acid promotes tissue repair, it can shorten wound healing time and reduce scar formation. Many clinical studies have reported such effects of hyaluronic acid. In the healing of 21 wounds caused by erbium laser, the wounds of subjects treated with oat Rhealba extract and high-molecular-weight hyaluronic acid formulations healed within 9 days, while the control group treated with panthenol and hydroxyproline formulations also healed within 9 days. while those treated with resveratrol copper healed in 12 days, and the untreated control group healed in 16 days. The hyaluronic acid group showed a significant reduction in healing time [17]. In a clinical trial involving 60 cases of local burns (average burn area approximately 3% of body surface area) treated with a high-molecular-weight hyaluronic acid zinc gel, wound size reduced to 50% of the original wound size by day 5, 93.3% of participants achieved complete epithelialisation by day 21, and 91.7% of participants experienced pain relief by day 10. No wound infections occurred during the wound healing process [18].
In a controlled experiment involving 30 cases of second-degree burn healing, olive oil and high-molecular-weight hyaluronic acid had similar effects on burn healing time, but olive oil was more effective in preventing scar formation [19]. In a randomised clinical trial comparing the topical application of high-molecular-weight hyaluronic acid and a neutral medium on 89 cases De piernaVenoso venosoulcers, the results showed that by day 45, the ulcer healing area was significantly larger in the hyaluronic acid group compared to the control group (hyaluronic acid group: 73.4 ± 4.6% vs. control group: 46.9 ± 9.6%, P = 0.011), and the number of healed Úlceras úlceras.at 45 and 60 days was significantly higher than that in the control group (45 days: hyaluronic acid group 31.1% vs. control group 9.3%, P = 0.011) (60 days: hyaluronic acid group 37.8% vs. control group 16.3%, P = 0.024) [20].
3.3 Terapia de barrera para la enfermedad
Studies have shown that impaired epidermal barrier function plays a significant role in the development of atopic dermatitis and other allergic diseases, and dry skin is more prone to eczema. The addition of moisturisers containing hyaluronic acid can improve the integrity of the stratum corneum. Some studies have shown that barrier therapy can reduce the frequency and severity of skin disease flare-ups and decrease the need for topical corticosteroids or topical calcineurin inhibitors. Among these, hyaluronic acid may play a crucial role in the epidermis' Respuesta natural al trauma, incluyendo migración de queratinocitos en la dermatitis atópica y proliferación celular durante la cicatride heridas y reparación de barrera [21].
Palmer et al. [22] conducted a randomised controlled trial to evaluate the efficacy and seguridadof MAS063D (a cream containing high-molecular-weight hyaluronic acid) in treating 30 patients with atopic dermatitis. After two weeks of treatment, MAS063D significantly reduced the itch severity index (EASI) in patients; Draelos et al. [23] conducted a controlled trial comparing a 1% high-molecular-weight hyaluronic acid-based pimecrolimus gel with a medicinal ceramide cream in the topical treatment of atopic dermatitis. At the start of the experiment, and at weeks 2 and 4, patients were assessed for erythema, crusting, lichenification, skin peeling, itching, stinging, and burning. At week 2, patients in the hyaluronic acid group showed significant improvement in eczematous lesions compared to the control group, but there was no significant difference in lesion recovery by week 4. Hyaluronic acid-based formulations are easier to apply and absorb than traditional drugs and have a milder odour, improving patient compliance. However, this study had a small sample size, no control group was established, and an appropriate assessment sylowas lacking, necessitating further experiments to support these results [24].

3.4 enfermedades inflamatorias
The anti-inflammatory regulatory mechanisms of hyaluronic acid have been demonstrated in some drug delivery media, skin barrier function repair, and wound healing. Additionally, topical hyaluronic acid has shown efficacy in treating facial seborrheic dermatitis. However, in in vitro experiments on inflammation regulation, small-molecule hyaluronic acid often exhibits pro-inflammatory effects (as described in Section 2.3), so the mechanism of topical hyaluronic acid in treating inflammatory diseases remains unclear. The main drugs used for facial seborrheic dermatitis are corticosteroids and antifungal agents, but their application is limited due to adverse reactions and drug sensitivity issues. A clinical trial by Schlesinger et al. [25] showed that topical application of 0.2% sodium hyaluronate improved symptoms such as erythema and itching in patients with facial seborrheic dermatitis. However, this clinical trial had a small sample size, and whether small-molecule hyaluronic acid regulates inflammation in a positive or negative manner remains controversial, so further clinical studies are needed to confirm its efficacy.
4 conclusión
Topical hyaluronic acid is safe and effective in dermatology. With the maturation of bacterial fermentation methods for Producción de ácido hialurónicoSu bioseguridad se ha mejorado aún más, y los costos de producción han disminuido en comparación con los métodos anteriores. Esto lo hace más adecuado para aplicaciones tópicas. Con el continuo desarrollo de la biotecnología, la aparición de nuevos materiales como las micelas poliméride de nanopartículas puede permitir que el ácido hialurónico exhimejores propiedades fisicoquímicas para uso tópico en dermatología.
In many skin lesions, such as psoriasis, the normal hyaluronic acid reticular structure is partially missing in the spinous layer and granular layer, and hyaluronic acid is present in the stratum corneum of dyskeratosis. Whether correcting the abnormal distribution of hyaluronic acid in the epidermis of psoriasis patients can improve the symptoms of related skin diseases is worthy of further study. Studies have shown that with the increase of age, the expression of hyaluronic acid and CD44 receptor in the skin showed a downward trend. At this time, the role of exogenous hyaluronic acid in various aspects was weakened, so whether there were differences in the dosage and frequency of use at different ages is still worth discussing. Because hyaluronic acid exerts its antioxidant effect through its own degradation and ROS elimination mechanism, its application in anti-aging drugs is worth tracking.
referencia
[1] Liang J,Jiang D,Noble PW. hialuronan as a Terapéutica terapéutica terapéutica terapéutica terapéutica El objetivo Enfermedades [J]. Adv La droga Comisión Rev,2016, 97:186-203.
[2]Stern R,Asari AA,Sugahara KN. Hyaluronan fragments: an information-rich system (en inglés). Eur J Cell Biol,2006,85 (8) : 699-715.
[3] Nowacki M,Pietkun K,Pokrywczyńska M,et al.rellenar efectos, persistencia, y safety Fabricación a Productos de relleno Formulado con stem Células células En un modelo animal [J]. t Surj, 2014,34(8) : 1261-1269.
[4]DeLorenzi c.degradación transarterial del ácido hialurónico por hialuronidasa [J]. Dermatol Surg,2014,40(8) : 832- 841.
[5]Zhao N,Wang X,Qin L,et al.efecto del peso molecular Y concentración de hialuronano sobre la proliferación celular y la diferenciación so - teogénica in Vitro [J]. Biochem Biophys Res Commun,2015,465(3) : 569-574.
[6] Slevin M,Kumar S,Gaffney j.angioligosacáridos of hialuronan induce múltiples señalización Caminos caminos en Células endotelivasculares mitogéy cicatride heridas respon- ses[J]. J Biol Chem,2002,277(43) : 41046-41059.
[7] Komorowicz E, Balazs N,Varga Z,et al.hyalurronic acid Disminuye la estabilidad mecánica, pero aumenta la resistencia lítica de las matrices de fibrina [J]. Matrix Biol,2017,63:55-68.
[8]Petrey AC,de la Motte CA.Hyaluronan, un regulador crucial de la inflamación [J]. Front Immunol,2014,5:101.
[9]Naor D.Editorial: interacción entre ácido hialurónico y sus receptores (CD44,RHAMM) regula the actividad Inflamación y cáncer [J]. Front Immunol,2016,7:39.
[10]Vigetti D,Karousou E,Viola M,et Al.Hyaluronan: bio- síntesis y señalización [J]. Biochim Biophys Acta,2014, 1840(8) : 2452-2459.
[11] Kim Y,Lee YS,Hahn JH,et al.hyalurronic acid targets (en inglés) CD44 e inhifcepsilonri señalización que implica PKCdel- ta,Rac1,ROS, y MAPK to ejercer antialérgico effect [J]. Mol Immunol,2008,45(9) : 2537-2547.
[12]Law CH,Li JM,Chou HC,et al.hyalurronic acid-depend- ENT Protección protección in H9C2 Cardiomiocitos: a cell modelo De isquemia y reperfusión cardilesión y tratamiento [J]. Toxi- cology,2013,303:54-71.
[13] Friedrich EE,Washburn NR.Transport patrones of anti - TNF- - - in burn wounds: Therapeutic implications of hyalu- (en inglés) Conjugación del ácido rónico [J]. Biomaterials,2017,114:10-22.
[14]Brown MB,Hanpanitcharoen M,Martin GP. Una investigación in vitro sobre el efecto de los glucosaminoglicanos en la piel Partipartición y deposición of AINE [J]. J Pharm, 2001,225(1-2) : 113-121.
[15]Gupta AK,Paquet M,Villanueva E,et al.Interventions for Queratosis actínica [J]. Cochrane Cochrane Base de datos Syst Rev,2012, 12.
[16] Mejkalova D,Muthn → T, Neporova K,et al.micelas polimérihialuronpara administración tópica de fármacos [J]. Carbohydr Polym,2017,156:86-96.
[17]Sabadotto M,Theunis J,Black D,et al.evaluación in vivo del efecto de una crema que contiene Avena Rhealba( ) y ácido hialurónico en la piel deepidermizada producida con un erbium-YAG Láser [J]. Eur J Dermatol,2014,24(5) : 583-588.
[18] juhász I,Zoltán P,Erdei i.tratamiento de quemaduras de espesor parcial con Zn-hyaluronan: lecciones de un estudio clínico piloto [J]. Ann Burns Fire Disasters,2012,25(2) : 82-85.
[19]Campanati A,De Blasio S,Giuliano A,et al.tópico ozon- ated Oil versus hialurónico gel para el tratamiento De partial-to De espesor total Segundo grado Quemaduras: Ensayo clínico prospectivo, comparativo, ciego sencillo,no aleatorizado, controlado Trial [J].Burns,2013,39(6) : 1178-1183.
[20]Humbert P,Mikosinki J,Benchikhi H,et al.Efficacy and Seguridad de una almohadilla de gasa que contenga ácido hialurónico en el tratamiento of leg ulcers of venous or Origen mixto: a Doble ciego, Alealeatori, controlados Trial [J]. En el Herida herida J,2013,10 (2) : 159-166.
[21]Maytin EV,Chung HH,Seetharaman VM. Los hialurónicos participan en la respuesta epidérmica a la interrupción de la barrera de permeabilidad in vivo[J]. Am J Pathol,2004,165 (4) : 1331-1341. [22]Palmer CN,Irvine AD,Terron-Kwiatkowski A,et al.Com- mon pérdida de función las variantes de la barrera epidérmica pro- tein filaggrin son un factor predisponimportante para der- matitis atópica [J]. Nat Genet,2006,38(4) : 441-446.
[23]Draelos ZD. Una evaluación clínica de la eficacia comparable Espuma a base de ácido hialurónico y crema de mezcla que contiene cera en el tratamiento de los atópicos leves a moderados Dermatitis [J]. J Cosmet Dermatol,2011,10(3) : 185-188.
[24]Frankel A,Sohn A,Patel RV,et al.estudio de comparación bilateral de unungüento de pimecrolimus al 1% y una espuma emoliente de ácido cerami-hialurónico en el tratamiento de pacientes con dermatitis atópica [J]. J Drugs Dermatol,2011,10(6) : 666-672.
[25]Schlesinger T,Rowland PC. Eficacia y seguridad de un gel tópico de ácido hialurónico de bajo peso molecular en el tratamiento de la dermatitis seborreica facial informe final [J]. J esur Dermatol,2014,7(5) : 15-18.
-
anterior
¿Cuál es el uso de ácido hialurónico en el producto de cuidado facial?
-
siguiente
¿Cuál es el uso del ácido hialurónico en el campo Oral?


 inglés
inglés francés
francés español
español ruso
ruso coreano
coreano Japonés japonés
Japonés japonés




