¿Cuáles son los usos clínicos del ácido hialurónico?
The unique physical ychemical properties ymultiple physiological functions deÁcido hialurónicohave found widespread application enmedicine ybiomaterials. In el1960s, Balazs [1] first used hialurónicaÁcido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácidoin complex retinal detachment surgery, achieving significant therapeutic effects; in el1970s, hyaluronic acid preparations began abe applied in joint diseases; in the 1980s, hyaluronic acid emerged in the field deaesthetics. Since then, hyaluronic acid has been increasingly applied in ophthalmology, orthopaedics, dermatology, cosmetic surgery, and other Quirúrgicunquirúrgicafields, conrapid advancements in related research.
1 propiedades físicas y químicas y efectos fisiológicos
In 1934, Professors Meyer and Palmer from the Department deOphthalmology at Columbia University in the United States first isolated hyaluronic acid (HA) from the vitreous humour decow eyes. In 1937, Kendell and others extracted this active substance from bacteria [2]. In 1950, Karl Meyer&#El laboratorio 39;s diludilucidó con éxito la estructura química del ácido hialurónico [3]. El ácido hialurónico es un polímero de alto peso molecular, con las unidades estructurales básicas siendo el ácido d-glucurónico y la n-acetil-d-glucosamina, Unidos alternando enlaces glicosídicos − 1,3 y − 1,4. Debido a la presencia de grupos carboxilo ácidos, el ácido hialurónico se disodifica fácilmente en solución de clorsódico, liberando H+ y adoptando un estado de catión poliiónico ácido [4], lo que confiere sus propiedades de mucopolisacárido ácido.
hialurónicaacid is widely distributed in the connective tissues deliving organisms, such as the umbilical cord, cartilage, vitreous humour dethe eye, blood vessel walls, joint fluid, and skin [5]. In biological organisms, hyaluronic acid exhibits various physiological activities, including lubricating joints, regulating protein activity, inhibiting microbial invasion and the spread of toxic substances, promoting wound healing, and regulating vascular wall permeability [6].
2 aplicaciones clínicas en cirugía
2.1 tratamiento de las enfermedades articulares
Hyaluronic acid is commonly found in synovial fluid in the form of sodiosalts, with Hialuronato de sodiobeing the primary component of synovial fluid and also a component of cartilage matrix [7]. It plays a lubricating role within the joint cavity, reducing friction between connective tissues; simultaneously, it exerts elastic properties to cushion external forces exerted on joint cartilage. Injecting high-molecular-weight, high-concentration, and high-viscoelastic sodium Hialuronato de hialuronatointo the joint cavity can enhance the viscosity and lubricating function of synovial fluid, protect joint cartilage from further damage, and promote the healing and regeneration of joint cartilage, significantly alleviating pain and improving joint mobility [8].
Knee osteoarthritis: Bannuruet al. [9] published a Revisión sistemáticain 2011, which included 54 high-quality clinical alealealecontroladaEnsayos clínicos(RCTs) involving 7,545 participants. The trial design compared hyaluronic acid with placebo parathe treatment of knee osteoarthritis, administered via intra-articular injection, with the primary outcome being the reduction in pain response. Meta-analysis results showed that treatment began to show efficacy después4 weeks, reached maximum effect after 8 weeks, and the pain-relieving effect of hyaluronic acid persisted after 24 weeks. It was concluded that hyaluronic acid can serve as an effective drug parathe treatment of knee osteoarthritis.
Temporomandibular joint disorders: Manfrediniet al. [10] conducted a systematic review of hyaluronic acid treatment for temporomandibular joint disorders in 2010, including 19 clinical trials, of which 12 were for temporomandibular joint disorders and 7 for temporomandibular joint arthritis. The results showed that local injection of hyaluronic acid twice weekly significantly reduced pain compared with the placebo group, while joint function and mobility improved, but there was no difference in mouth opening size between the two groups; hyaluronic acid combined with aspiration was more effective than aspiration alone; and injection of hyaluronic acid in the lower part of the joint was more effective than in the upper part.

Ankle joint diseases: Loveday et al. [11] conducted a Cochrane systematic review on the intra-articular injection of hyaluronic acid for the treatment of ankle arthritis. This estudioincluded only one clinical trial with 15 participants, with a follow-up period of 6 months. All participants underwent arthroscopic minimally invasive surgery, followed by intra-articular injection of hyaluronic acid three weeks later. The results showed that hyaluronic acid did not have a significant advantage in pain relief but improved ankle joint mobility.
Shoulder joint diseases: Saito et al. [12] conducted a systematic review in 2010 on the efficacy and seguridadof hyaluronic acid shoulder injections for Crónica crónica crónica crónica crónicashoulder pain. A total of 19 RCTs and 2,120 participants were included. The results showed that hyaluronic acid injections into the shoulder effectively alleviated chronic shoulder pain and improved shoulder joint function, with no significant difference in the total number of adverse reactions between the two groups. This study also conducted a subgroup analysis comparing hyaluronic acid with corticosteroids, which showed that the hyaluronic acid group had better recovery of shoulder joint function than the corticosteroid group.
2.2 Para la reparación de heridas
El ácido hialurónico es uno de los principales componentes de la matriz extracelular en la epidery dermis de la piel humana [13]. Mejora las condiciones de crecimiento celular de la piel y proporciona un ambiente externo óptimo para la síntesis de colágeno y fibras elásticas en las células dérmicas [14]. También protege las células de tejido dañadas de bacterias patógenas, reduce las respuestas inflamatorias [15], mejora la cicatriy la regeneración de heridas, y acelera la regeneración del tejido de la piel.
Trauma repair: Voigt et al. [16] conducted a systematic review and meta-analysis of hyaluronic acid treatment for trauma in 2012. This study included 10 RCTs, 4 of which involved hyaluronic acid treatment for burns and 6 for ulcerated wounds. The results showed that hyaluronic acid accelerated wound healing in burn patients, shortened healing time, and higher concentrations of hyaluronic acid formulations were more beneficial for burn repair.

Postoperative wound repair: Metwally (en inglés)et al. [17] published a systematic review in 2007 on the use of hyaluronic acid solutions to prevent postoperative adhesionesafter gynaecological surgery, including 4 RCTs. The results showed that the incidence of adhesions was lower in the hyaluronic acid group than in the control group after gynaecological surgery; in Pacientes pacienteswho had developed adhesions, hyaluronic acid reduced the incidence of further adhesion progression, but there was no difference in the improvement rate of adhesions between the two groups. máset al. [18] published a systematic review in 2012, including five RCTs. The meta-analysis results showed that cross-linked hyaluronic acid Gel de gelreduces the incidence of adhesions after gynaecological surgery; in laparoscopic myomectomy, hyaluronic acid reduces the incidence of adhesions between the wound and the peritoneum; and in hysteroscopic gynaecological surgery, hyaluronic acid reduces the incidence of adhesions between the wound and the uterus.
2.3 Para enfermedades de la piel
Hyaluronic acid is the most effective natural moisturising agent discovered to date, possessing powerful water-binding and moisturising properties, capable of absorbing approximately 1,000 times its own weight in water. With age, nutritional deficiencies, sun exposure, environmental stressors, and other factors, the body's ability to synthesise hyaluronic acid gradually decreases, leading to a reduction in its concentration in the skin. This ultimately results in keratinisation, wrinkles, ageing, and even inflammatory reactions in the skin.
Actinic keratosis: Guptaet al. [19] published a systematic review in 2012, conducting a meta-analysis of various treatment measures for actinic keratosis. The study included three randomised controlled trials (RCTs) on hyaluronic acid treatment for actinic keratosis. The intervention in the treatment group was a 3% diclofenac sodium solution containing 2.5% hyaluronic acid, while the control group received a placebo. A total of 420 participants were included. The results showed that the efficacy rate in the treatment group was higher than that in the control group.
Radiación radiacióndermatitis: Kirova et al. [20] conducted a Fase faseIIIclinical trial usandoa randomised controlled blinded method to investigate the effect of hyaluronic acid on radiation dermatitis following radiotherapy for chest tumours. A total of 200 participants were included, with the intervention group receiving hyaluronic acid ointment and the control group receiving traditional moisturising ointment. The results showed that the incidence of radiation dermatitis was not significantly different between the two groups; however, the skin colour at the radiation site was better in the experimental group than in the control group. Additionally, the pain response in patients with radiation dermatitis was reduced after using hyaluronic acid cream. Pinnix et al. [21] conducted a randomised controlled clinical trial involving 130 participants. They compared the effects of hyaluronic acid gel and vaseline gel on the skin at the radiation site in female Seno (mama).Cáncer de cáncerpatients undergoing radiotherapy. Applied hyaluronic acid gel versus vaseline gel to the irradiated areas. Results showed that hyaluronic acid did not reduce the incidence of grade 2 or higher radiation dermatitis.

Scleroderma: Yu Chunshui et al. [22] investigated the treatment of advanced localized scleroderma, enrolling 22 patients with scleroderma. Participants were randomly assigned to two groups: the experimental group (11 patients) received hyaluronic acid spot injections once every 5 weeks for a total of 15 weeks, while the control group (11 patients) received hyaluronic acid spot injections once weekly for a total of 15 weeks. At the end of week 15, the efficacy rate in the experimental group was 90.91%, while in the control group it was 45.45%. One adverse reacciónoccurred in the experimental group and three in the control group, all manifesting as swelling at the injection site. The results indicate that hyaluronic acid is safer and more effective than hyaluronidase for the treatment of scleroderma.
Skin rejuvenation: Narins et al. [23] selected 138 middle-aged and elderly female patients and conducted a comparative study on the efficacy of hyaluronic acid and collagen protein subcutaneous injections for the removal of nasolabial folds. The injection frequency was once every 2 weeks until the nasolabial folds faded to a satisfactory effect, with a maximum treatment duration of 6 months. The results showed that after 6 months, the efficacy rate for fading nasolabial folds was 59.6% in the hyaluronic acid group and 9.5% in the collagen group; among those who achieved satisfactory results, the number of injections required was fewer in the hyaluronic acid group than in the collagen group; there were no significant differences in post-injection reactions or tolerability between the two groups.
2.4 Aplicaciones en enfermedades oftálmicas
Sodium hyaluronate is an important component of aqueous humour and vitreous humour, protecting the corneal endothelium, iris, and retina [24]. Injection of sodium hyaluronate into the anterior chamber maintains anterior chamber depth; injection into the vitreous cavity aids in retinal repositioning; and in ophthalmic surgery, it reduces intraoperative or postoperative adhesions. Hyaluronic acid can also adsorb and bind large amounts of water molecules, preventing ocular dryness, and is used for corneal damage caused by or associated with dry El ojosyndrome, intrinsic disorders, or external stimuli [25].
Dry eye disease: McDonald McDonaldet al. [26] selected 39 patients with dry eye disease and conducted a randomised crossover controlled trial to compararthe therapeutic effects De 0,1%sodium hyaluronate and polyvinyl alcohol. A total of 32 patients completed the entire two-way crossover trial. Both groups received local topical instillation three to four times daily. After four weeks of treatment and control measures, the groups were crossed over and treated for another four weeks. The results showed that the burning sensation was significantly lower in the hyaluronic acid group than in the polyvinyl alcohol group, and the recovery of corneal function was better in the hyaluronic acid group than in the polyvinyl alcohol group (P = 0.04 < 0.05).
Queratitis: Liu Jun [27] publicó un ensayo clínico controlado aleatorizado en 2011 que investigel tratamiento de la queratitis por el virus del herpes simple con ácido hialurónico. Se incluyeron un total de 26 sujetos, 14 en el grupo de tratamiento y 12 en el grupo de control. Las medidas de tratamiento para el grupo de tratamiento fueron0,1% gotas de ácido hialurónicoCombinado con ungüento de ganciclovir, mientras que el grupo de control recibió gotas oftálmicas de Tylenol combinadas con ganciclovir. Los resultados mostraron que las gotas oftálmicas de ácido hialurónico podrían acortar el tiempo de cicatridel epiteliy mejorar la agudevisual en pacientes con queratitis por herpes simple epiteli.
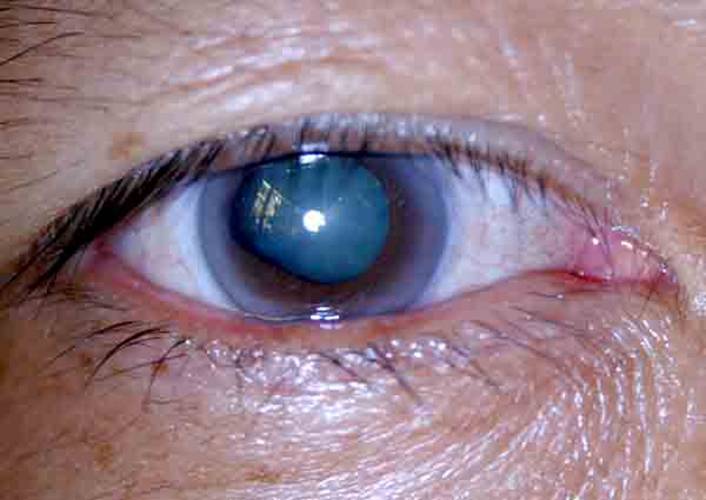
Low intraocular pressure: Kucukerdonmez et al. [28] conducted a clinical study on the treatment of chronic low intraocular pressure with hyaluronic acid, enrolling 32 patients with low intraocular pressure, with an average age of 56.8 years. The treatment involved intravitreal injection of sodium hyaluronate. After treatment, patients recovered well, indicating that hyaluronic acid is effective for treating low intraocular pressure.
Eye burns: Zhao Fajun et al. [29] treated patients with eye burns using traditional methods such as erythromycin or tetracycline eye ointment, chloramphenicol eye drops, and atropine for mydriasis when necessary. Additionally, they administered 0.1% sodium hyaluronate eye drops combined with 2% ofloxacin eye drops every 4 hours. Results showed that early application of sodium hyaluronate after eye burns reduced severe complications and disability rates.
2.5 otros
Ye Shufen [30] and Lai Hanbiao et al. [31] reported that the use of hyaluronic acid gel after dental implant surgery effectively reduces pain responses and alleviates redness and swelling. Wu et al. [32] and Wang Jianping et al. [33] found that hyaluronic acid administered to patients after dacryocystitis surgery promotes the recovery of lacrimal sac function and reduces postoperative scarring.
Referencias:
[1]Karen LG, Paul B. Hyaluronic Acid [J]. Drogas, 1994, 47(3): 536-566.
[2]Liu Zhengping, Wang Bing. Avances en investigación clínica en ácido hialurónico [J]. Food and Medicine, 2006, 8(12A): 8-10.
[3]Weissmann B, Meyer K. la estructura del ácido hialobiurónico y del ácido hialurónico del cordón umbilical [J]. J Am Chem Soc, 1954, 76(7): 1753-1757.
[4]Cui, Yuan, Duan, Qian y Li, Yanhui. Progreso de la investigación sobre el ácido hialurónico [J]. Journal of Changchun University of Science and Technology: Natural Science Edition, 2011, 34(3): 101-106.
[5] Liu L,Liu Y,Li J,et al.Microbial production of hyaluronic acid: current State,challenges,and Perspectives [J]. Hecho de células Microb,2011,10(99) : 1-9.
[6] Iannitti T,Lodi D,Palmieri B. inyecciones intraarticulares para el tratamiento de la osteoartritis: enfoque en el uso clínico del ácido hialurónico [J]. Drugs R D,2011,11(1) : 13-27.
[7]Wobig M,Dickhut A,Maier R, et al.viscosupplement with Hylan G - F 20: un ensayo controlado de 26 semanas de eficacia y seguridad en la rodilla osteoartrítica [J]. Clin Terapeut,1998,20(3) : 410-423.
[8] Brandt KD, bloque JA,Michalski JP. Eficacia eficacia and safety Fabricación a Hialuronato de sodio en osteoartritis de rodilla [J]. Clin Orthopaed Res relacionados, 2001,385: 130 — 143.
[9] Bannuru RR, Natovz NS,Dasi UR, et al.trayectoria terapéutica tras inyección intraarticular de ácido hialurónico en artrode rodilla e meta - Análisis [J]. Osteoosteoy cartílago,2011,19(6) : 611-619.
[10] Manfredini D,Piccotti F,Guarda-Nardini Ácido hialurónico en el tratamiento de las afecciones de la articulación temporomandibular: una revisión sistemática de la literatura [J]. The Journal of Craniomandibular Practice,2010,28(3) : 166 -176.
[11]Loveday D,Clifton R, Robinson A. intervenciones para el tratamiento de defectos osteocondrales del Talus en adultos [J]. Cochrane Database of Systematic Re- views, publicado en línea en agosto de 2010. DOI: 10.1002/14651858. CD00 8104.
[12] Saito S,Furuya T,Kotake S.Therapeutic effects of hyaluronate in patients with chronic pain shoulder: a meta-meta-of random controlled trials[J]. Arthritis Care and Research,2010,62(7) : 1 009 - 1 018.
[13] Teh BM,Shen Y,Friedland PL,et al.Areview on the use of hyaluronic (en inglés) Ácido en la cicatride heridas de membrana timpánica [J]. Dictamen del experto Sr. Biol Ther, 2012,12(1) : 23-36.
[14] Dover JS,Rubin MG,Bhatia ac.revisión de los datos de eficacia, durabilidad y seguridad de dos rellende ácido hialurónico no estabilizado en animales a partir de un estudio prospectivo, aleatorizado, comparativo, multicéntrico [J]. Dermato- cirugía lógica,2009,35(1) : 322-331.
[15] Stegmann R, Miller d.d.2 of Hialuronato de sodio en Traumatismo ocular penetrante grave [J]. Ann Ophthalmol,1986,18(1) : 9 — 13.
[16]Voigt J, conductor VR. Derivados del ácido hialurónico y su efecto curativo sobre las quemaduras epiteliales surgical Heridas, y chronic Heridas: a systematic review and meta-análisis of Aleatoriatorio o controlled trials [J]. Reparación y regeneración de heridas,2012,20(3) : 317 -331.
[17] Metwally M,Gorvy D,Watson A,et al.Hyaluronic Agentes fluidos ácidos para el Prevención prevención of adhesions after Conservación de fertilizantes Cirugía ginecológica: un meta-análisis de ensayos controlados aleatorios [J]. Fertilidad y esterilidad,2007,87(5) : 1 139 -1 146.
[18] Mais V,Cirronis MG,Peiretti M,et al.Efficacy of Auto-crosslinked hyaluronan gel for adhesion Prevention in laparoscopy and hysteroscopy: a systematic review and meta-analysis of random controlled trials[J] (en inglés). European Journal of Obstetrics and Gynecology and Reproductive Biolo- Gy,2012,160(1) : 1-5.
[19] Gupta AK,Paquet M,Villanueva E,et al.Interventions for actininic ker- atoses[J]. Cochrane Database of Systematic Reviews, publicado en línea: Diciembre de 2012. DOI: 10.1002/14651858.CD004415.
[20]Kirova YM,Fromantin I,De Rycke Y,et al.Can we the skin re- action in breast cancer patients using hyaluronic acid Durante la radiación ¿Terapia? resultados of phase III randomised Trial [J]. otros Oncol, 2011,100(2) : 205-209.
[21]Pinnix C,Perkins GH,Strom EA,et al.tópico Hyaluronic Ácido vs.estándar of Cuidado de la prevención of Radiation Dermatitis tras adyuv Radioterapia radioterapia for Seno (mama). Cáncer: Ventanilla única Ensayo clínico aleatorizado de fase III [J]. International Journal of Radiation Oncology Biology Physics,2012,83(4) : 1 089 -1 094.
[22] Yu Chunshui, Ran Liwei, Tan Shengshun, et al. Análisis de eficacia de la inyección local de hialuronato de sodio e hialuronidasa en el tratamiento de la esclerodermia localizada en estadio tardí[J]. Chinese Journal of Dermatology, 2006, 20(1): 26-28.
[23] Narins RS,Brandt F,Leyden J,et al.una comparación aleatori, doble ciego,mul- ticenter de la eficacia y tolerabilidad de Restylane versus Zy- plast para la corrección de pliegues nasolabiales [J]. dermatdermatsurgery: offi- cial publication for American (en inglés) Sociedad de la Dermatologic Cirugía,2003, 29(6) : 588-595.
[24] Algawi K,Agrell B,Goggin M,et al.ensayo clínico aleatoride tópico Hialuronato de sodio después de la queratectomía fotorrefraccon láser excimer [J]. J Refract Surg,1995,11(1) : 42-44.
[25] Faraldi F,Papa V,Santoro D,et al.A Nuevo nuevo eye gel containing sodium hyaluronate and « Goma de goma for the gestión De abrasiones cornepostraum[J]. Journal of Clinical Ophthalmology,2012,6: 727 - 731.
[26] McDonald CC,Kaye SB,Figueiredo FC,et al.A centro study to compare the rendimiento of 0.1% (w/v) sodium hyaluronate with 1,4% (w/v) Alcohol polivinílico en el alivio de Síntomas asociados con el síndrome de ojo seco [J]. Eye (Londres, Inglaterra), 2002,16(5) : 601-607.
[27]Liu Jun. efecto de las gotas de hialuronato de sodio en la cicatriepitelien la queratitis por el virus del herpes simple [J]. Huaihai Medicine, 2011, 29(6): 522-523.
[28]Kucukerdonmez C, Beutel J, Bartz-Schmidt KU, et al. Tratamiento de la hipotonía ocular crónica con aplicación intraocular de hialuronato de sodio [J]. British Journal of Ophthalmology, 2009, 93(2): 235-239.
[29]Zhao Fajun, Zong Xiao. Observación sobre la eficacia del hialuronato de sodio en el tratamiento de quemaduras químicas del ojo [J]. Medical Theory and Practice, 2007, 20(1): 69-70.
30 vosotros sujéfen. El papel de gel de ácido hialurónico en la cicatride heridas después de cirugía de implante [J]. International Journal of Medicine and Health, 2006, 12(7): 34-35.
[31]Lai janbiao, Liu Yi. El papel del gel de ácido hialurónico en la cicatride heridas después de cirugía de implantes [J]. Guangdong Journal of Stomatology, 2008(16): 637-638.
[32]Wu W, Cannon PS, Yan W, et al. Efectos de la cobertura de Merogel sobre la cicatride heridas y la patencia ostial en dacriocistorrinostomía endoendonasal para dacriocistitis crónica primaria [J]. Eye (Lond), 2011, 25(6): 746-753.
[33]Wang Jianping, Zhang Deshou, Ma Yong, et al. Aplicación de hialuronato de sodio en la anastomosis nasolacrimal [J]. International Journal of Ophthalmology, 2009, 24(6): 3828-3829.
-
anterior
¿Cuáles son los usos del polvo de ácido hialurónico en la osteoartritis?
-
siguiente
¿Cuáles son los usos del polvo de ácido hialurónico en el campo de la alimentación?


 inglés
inglés francés
francés español
español ruso
ruso coreano
coreano Japonés japonés
Japonés japonés





