Exploring Hyaluronic Acid Powder for Bone Tissue Health Solutions
Ácido hialurónico, asunnatural biomaterial with outstanding properties, demonstrates significant applicatielpotential enelfield deboneTejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejidorepair materials. Its unique physicochemical characteristics align closely with the requirements paraideal bonescaffold materials, providing a crucial directielfor the design ydevelopment of next-generation bone repair materials.
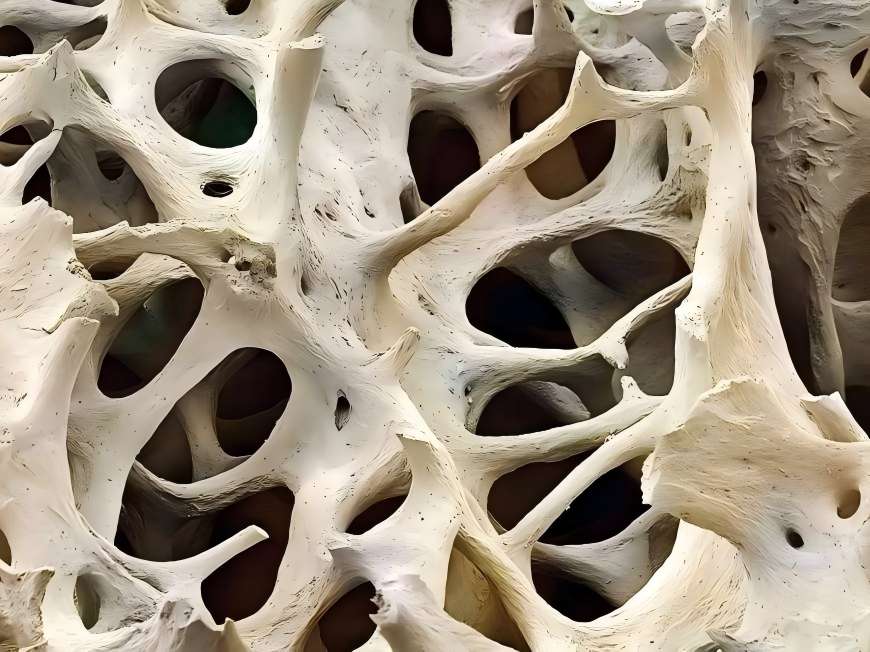
An ideal bone Tejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejido tejidoengineering scaffold must possess excellent biocompatibility, controlled degradability, a three-dimensional porous structure, ysurface properties conducive to cell adhesion ygrowth. Ácido hialurónico powder not only exhibits outstanding viscoelasticity, plasticity, and high water absorption but also demonstrates excellent biocompatibility and non-immunogenicity, providing Células célulaswith a suitable microenvironment. Through molecularmodification and material composites, its mechanical strength, pore structure, and degradation properties can be further optimised to better meet the physical and biological requirements for bone tissue repair.
Moreover, hialurónicaacid-based materials exhibit favourable processability, enabling the formation of three-dimensional scaffolds with interconnected porous networks through various advanced fabrication techniques. This facilitates cell migration, nutrient delivery, and vascular ingrowth. These properties render hialurónicaÁcido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácidoan ideal candidate for developing bioactive bone repair materials, offering broad prospects for innovative applications in tissue engineering.
1 Innovative Applications of Hyaluronic Acid: Molecular Properties Empowering New Directions in Joint Health Material Development
As a natural biopolymer, Polvo de ácido hialurónico exhibits multifaceted advantages in biomaterials for joint health. Its unique molecular structure and physicochemical properties have garnered significant attention across diverse biomaterial applications.
Research indicates that hyaluronic Ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácido ácidoforms complexes with proteins within the joint environment, exhibiting excellent water absorption, viscoelasticity, and lubricating properties. These characteristics enhance the rheological behaviour of materials and their affinity for biological interfaces, demonstrating positive effects on extracellular matrix composition and metabolic environments in vitro models.
Moreover, hyaluronic acid powder exhibits favourable biocompatibility and molecular integration capabilities. Its polymeric network structure assists in maintaining microenvironmental stability while providing conducive conditions for cellular metabolism. These properties furnish robust scientific foundations for developing advanced hyaluronic acid-based biomaterials, particularly demonstrating broad prospects in joint health-related applications.
2 Breakthrough Innovations in Hyaluronic Acid-Based Composites Empower New Developments in Bone Tissue Engineering
Recently, innovative biomaterials based on hyaluronic acid have emerged as a research hotspot in bone tissue engineering. Leveraging its outstanding biocompatibility, degradability, and modifiability, hyaluronic acid, through advanced cross-linking and modification techniques, has significantly enhanced mechanical strength, structural stability, and functional diversity, offering novel approaches for designing next-generation biomaterials.
Crosslinking modification, as a core technique, introduces multiple functional groups to form three-dimensional network structures within hyaluronic acid molecules. This not only prolongs the material's functional duration but also substantially mejoraits mechanical properties and resistance to degradation. Currently, diverse modified hyaluronic acid materials have emerged in scientific research, including aminopropyl glycerol crosslinked derivatives, photopolymerisable hyaluronic acid, and esterified hyaluronic acid benzyl esters. These materials demonstrate promising potential in cellular affinity, sustained-release properties, and carrier functionality.
Modified hyaluronic acid-based composites achieve a leap in mechanical properties and stability while preserving the biocompatibility of the natural material, greatly expanding their application prospects as tissue engineering scaffold materials. Such materials are expected to provide more reliable and efficient solutions for bone repair, driving the development of regenerative medicine materials towards high performance and functionalisation.
Industry experts indicate that with continuous advancements in material modification techniques and deepening applied research, hyaluronic acid-based composites are poised to play increasingly significant roles in biomaterials manufacturing, tissue engineering, and healthcare sectors, delivering a series of innovative productsAl mercado.

3 Breakthrough in Hyaluronic Acid Composites: Pioneering a New Era in Bioactive Factor Delivery
Significant progress has recently been made in the development of hyaluronic acid-based biomaterials. Leveraging its exceptional carrier properties and modifiability, hyaluronic acid has emerged as a core material for bioactive El factordelivery systems, continually expanding its application boundaries through innovative molecular modification techniques.
Optimising material properties has become a current research focus. Studies indicate that covalently bonding hyaluronic acid with specific biological ligands significantly enhances its cell adhesion properties and factor loading capacity. The newly developed hyaluronic acid-integrin composite hydrogel system demonstrates outstanding biofactor loading and sustained-release characteristics, offering innovative insights for next-generation biomaterial design.
Industry experts note that such composite materials synergistically enhance performance by effectively integrating the advantages of diferentessubstances. This not only broadens hyaluronic acid's application scenarios but also provides novel technical solutions for tissue engineering and regenerative medicine. Current R&D efforts are increasingly focused on optimising the materials' biocompatibility, degradation characteristics, and structural stability to accelerate their industrialisation.
Looking ahead, with continuous advancements in surface modification techniques and materials engineering, functionalised hyaluronic acid-based composites are poised to become a significant innovation platform within the biopharmaceutical sector, delivering further breakthrough products to the industry.
4 perspectivas
Hyaluronic acid powder, as a naturally biodegradable biomaterial, has become a crucial foundational material in bone tissue engineering due to its outstanding biocompatibility, hydrophilicity, and three-dimensional network structure. Primavera verde Technology leverages advanced biological extraction and modification techniques to provide clients with high-quality hyaluronic acid powder solutions, supporting the development of next-generation bone repair and regenerative medicine products.
Green Spring Technology's hyaluronic acid raw materials offer the following advantages:
· Outstanding biocompatibility and controllable degradability, providing an optimal growth microenvironment for cells;
· High hydrophilicity and porous structure, supporting cell adhesion, proliferation, and directed differentiation;
·Exceptional structural plasticity, enabling its use as a functional scaffold material providing temporary support for tissue regeneration;
·Non-immunogenic and highly safe, suitable for high-end biomedical applications.
Green Spring Technology remains committed to supplying stable, compliant, and customizable high-purity hyaluronic acid raw materials, empowering product innovation and jointly advancing progress in regenerative medicine. Contact us now at helen@greenspringbio.com or WhatsApp: +86 13649243917 for detailed product specifications, application case studies, and quotations.
referencia
[1]Silber JS,Anderson DG,Daffner SD,et al anterior ilíilíilíilíilíilíilíilí crest bone La cosecha for De un solo nivel Discectomía cervical anterior y Fusion [J]. Spine,2003,28 : 134 - 139.
[2]Salgado AJ,Coutinho OP, RL. Bone tissue Ingeniería: estado del arte y tendencias futuras [J]. Macromol Biosci,2004,4:743-765.
[3]O'Brien FJ. Biomaterials & scaffolds for tissue (en inglés) Ingeniería [J]. Materiales hoy,2011,14(3) : 88-95.
[4]Bae MS,Yang DH,Lee JB,et al.base de ácido hialurónico fotocurado hidrog« Que contengan simvastatina as a bone tissue Andamio de regeneración [J]. Biomaterials,2011,32 (32) : 8161- 8171.
[5]Manicourt DH, Pita JC, Thonar EJ. Proteoglicanos no dissciativamente extraídos desde different zonas of Cartílago canino normal [J]. Connect Tissue Res,1991,26 :231-246.
[6]Kawasaki K,Ochi M,Uchio Y. hialurónica acid enhances Proliferación proliferación and condrointinsulfato Síntesis síntesis síntesis in cultivada Condrocitos embeen gel de colágeno [J]. El papel de las 179:142 — 148.
[7] estufa J,Gerlach C,Huch K. Efectos de la proteoglicina hialuronana Contenido de condrocitos osteoartríin vitro[J]. J ortop Res, 2004,20(3) : 551-555.
[8]Kikuchi T,Yamada H,Fujikawa K. efectos De alto molecular peso hialuronan on the Distribución distribución distribución and movimiento De proteoglicano alrededor de condrocitos cultivados en cuentas de alginato [J]. Osteocartílago,2001,9(4) : 351-356.
[9]Huang Jianrong,Liu Shangli,Song Weidong,et al.insulinlike growth factor tipo 1 and hyaluronic acid on humana Embrión de cartílago articular cells fenotípica Efectos [J]. Diario de Sun Yat-sen University: Medical Sciences,2002,23 (6) :419-422.
[10]Baldini A,Zaffe D,Nicolini G. Defectos en los huesos Curación por alta - molecular hyaluronic Ácido :preliminar Resultados [J]. En Ann Stomatol: Roma,2010,1 (1) : 2-7.
-
anterior
How Hyaluronic Acid Elevates Your Cosmetic Formulations
-
siguiente
Precise Molecular Weight Control: Green Spring Hyaluronic Acid Drives Product Upgrades


 inglés
inglés francés
francés español
español ruso
ruso coreano
coreano Japonés japonés
Japonés japonés




